Clinical Application of Point-of-Care Gastric Ultrasound (POCUS) in Pre-Anesthetic Risk Assessment

1. Introduction: The Clinical Imperative
Pulmonary aspiration of gastric contents remains a significant and potentially devastating complication of anesthesia. Standard Nil Per Os (NPO) guidelines are the cornerstone of pre-procedural risk mitigation. However, these guidelines are a surrogate for true gastric volume and are frequently unreliable in specific patient populations.
Patients with comorbidities known to cause delayed gastric emptying—such as diabetic gastroparesis, neuromuscular disorders, morbid obesity, and end-stage renal or hepatic disease—pose a heightened aspiration risk, even when NPO guidelines are reportedly followed. Furthermore, in emergency settings or cases with unclear fasting status, the clinician faces a critical knowledge gap.
Point-of-Care (POC) gastric ultrasound has emerged as an invaluable, non-invasive tool to objectively assess gastric content (both qualitative and quantitative), thereby refining aspiration risk stratification and informing anesthetic management.
2. Primary Objective: From “Uncertain NPO” to “Known Gastric Status”
The primary goal of pre-anesthetic gastric POCUS is to provide a real-time, objective evaluation of gastric volume and content at the bedside. This allows the anesthesiologist to move beyond assumption-based NPO status to a direct assessment, enabling evidence-based decisions regarding:
- The timing of elective surgery (proceed vs. delay).
- The selection of anesthetic technique (e.g., standard induction vs. Rapid Sequence Intubation (RSI)).
- The use of regional anesthesia as a primary modality to avoid airway instrumentation.
3. Sonographic Technique and Transducer Selection
Accurate assessment requires a systematic approach, typically focused on the gastric antrum, which serves as the most reliable window for evaluating gastric contents.
Transducer Selection:
- Low-Frequency (2-5 MHz) Convex Array Transducer: This is the standard probe for most adult patients. Its wide footprint and superior penetration depth are essential for identifying key anatomical landmarks (e.g., liver, aorta, inferior vena cava, and the gastric antrum itself), especially in patients with a larger body habitus.
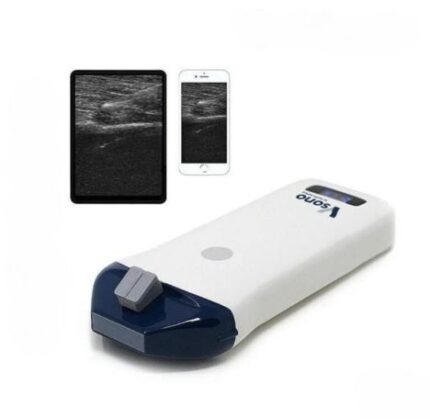
- High-Frequency (5-12 MHz) Linear Array Transducer: This probe offers superior spatial resolution at the expense of penetration depth. It is ideal for:
- Pediatric patients.
- Cachectic or very slim adult patients.
- Detailed evaluation of the gastric wall. In a truly empty, fasted state, the high-frequency probe can clearly delineate the five distinct sonographic layers of the gastric wall, which typically measures 4–6 mm in thickness.
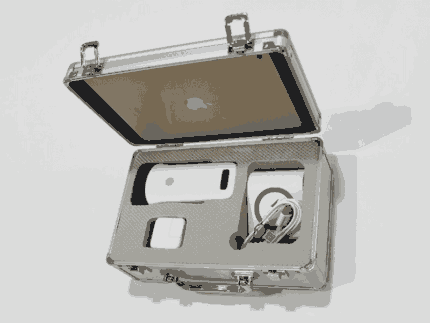
Dual-head wireless probes, which combine both a convex and linear transducer in a single device, offer flexibility in a POC setting, allowing the clinician to rapidly switch between deep anatomical surveys and high-resolution imaging.
4. Assessment Protocol and Interpretation of Findings
The assessment is dynamic, requiring scanning in at least two patient positions:
- Supine: The patient lies flat. This position allows for initial identification of the antrum, located between the left lobe of the liver and the pancreas.
- Right Lateral Decubitus (RLD): This is the most crucial position. Gastric fluid and contents pool dependently in the antrum, making them easier to identify and measure.
Qualitative Assessment (The Perlas Grading System):
This is the most common method for rapid risk stratification.
- Grade 0: Antrum is empty and appears flat or “target-like” in the RLD position. The walls are coapted. This signifies a truly empty stomach and minimal aspiration risk.
- Grade 1: Only clear, anechoic fluid is visible in the RLD position (but the antrum appears empty in the supine position). This is consistent with normal gastric secretions in a fasted state and represents a low aspiration risk.
- Grade 2: Clear, anechoic fluid is visible in both the supine and RLD positions. This indicates an expanded gastric volume (e.g., > 1.5 mL/kg) and is considered a high-risk “full stomach.”
- “Solid” or “Particulate” Stomach: The presence of hyperechoic, heterogeneous material (food particles) or a “frosted glass” appearance (particulate matter) indicates a non-fasted state, regardless of the patient’s position. This is an unequivocal high-risk finding.
Quantitative Assessment:
For a more objective measure, especially in Grade 2 findings, the antral cross-sectional area (CSA) can be measured in the RLD position. This measurement is then often used in established formulas to estimate the total gastric fluid volume.
- Formula: Gastric Volume (mL) = [Customary formula, e.g., 27.0 + 9.5 * (RLD CSA in cm²)] (Note: Various formulas exist and institutional protocols may differ).
- Clinical Cutoff: While debated, a clear fluid volume of < 1.5 mL/kg is generally accepted as a low-risk threshold.
5. Clinical Integration and Conclusion
Gastric POCUS is a rapid, reliable, and teachable skill that significantly enhances the anesthesiologist’s pre-operative assessment. It provides objective, actionable data that can validate or invalidate a patient’s NPO status. In high-risk populations, its routine use can lead to a demonstrable reduction in aspiration risk by guiding appropriate modifications to the anesthetic plan, thereby moving patient safety from a protocol-based assumption to an evidence-based certainty.