Guidance for Peripheral Nerve Blocks
Revolutionizing Pain Management: Advanced Ultrasound Guidance for Peripheral Nerve Blocks
Introduction to Ultrasound-Guided Peripheral Nerve Blocks
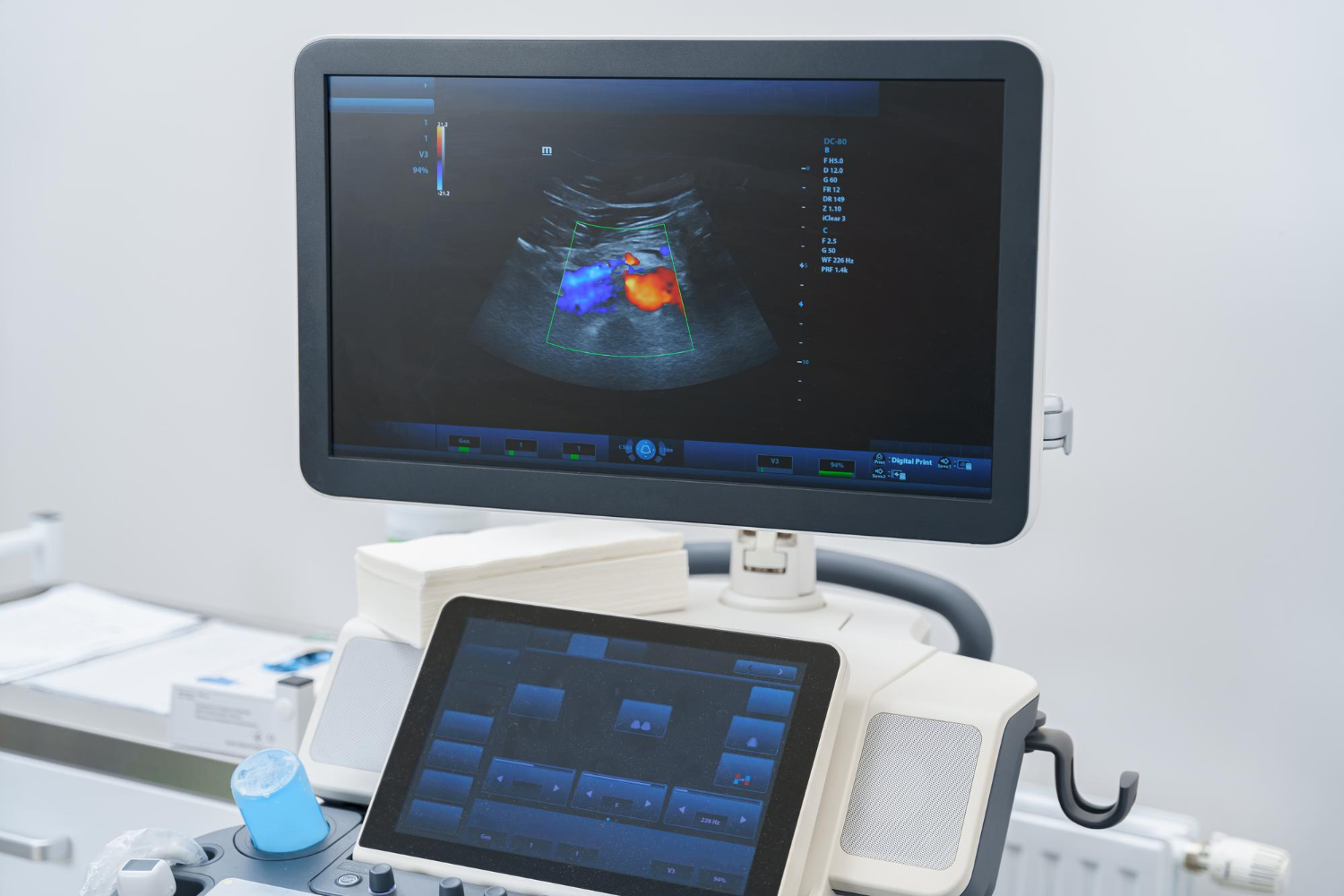
Peripheral nerve blocks (PNBs) represent a cornerstone of modern anesthesia practice, providing targeted pain relief for surgical procedures while avoiding systemic side effects of general anesthesia. The integration of ultrasound (US) guidance has transformed PNB from a landmark-based technique to a precision-based intervention. By enabling real-time visualization of neural structures, surrounding tissues, and needle progression, ultrasound has elevated the efficacy and safety of regional anesthesia to unprecedented levels 19. This comprehensive review examines the clinical advantages of ultrasound-guided PNBs, explores technological innovations including Vendra Medical’s pioneering devices, and discusses emerging artificial intelligence applications that collectively enhance patient outcomes across diverse clinical scenarios.
Advantages of Ultrasound Guidance in PNB
1. Enhanced Precision and Efficacy
The dynamic visualization capabilities of ultrasound fundamentally differentiate it from traditional nerve localization methods. Unlike landmark-based techniques or nerve stimulation, ultrasound provides:
- Direct anatomical visualization: Practitioners can identify nerves through their echogenic signatures and spatial relationships to adjacent structures like blood vessels, muscles, and bones 19
- Real-time needle tracking: Continuous visualization of the needle tip prevents unintentional nerve contact and allows for precise local anesthetic deposition
- Controlled injectate spread: Observation of local anesthetic distribution ensures circumferential spread around target nerves, significantly improving block success rates 1
Clinical evidence demonstrates that ultrasound guidance achieves surgical anesthesia success rates of 72-98.8%, comparable or superior to nerve stimulation techniques (58-93.1%) 4. The technology particularly excels in deep nerve blocks (e.g., sciatic, lumbar plexus) where traditional methods face significant challenges 1.
2. Improved Safety Profile
Ultrasound guidance substantially mitigates risks associated with PNBs:
- Reduced complication incidence: Direct visualization decreases the likelihood of vascular puncture and hematoma formation 49
- Minimized nerve injury: Precise needle navigation prevents mechanical trauma while observation of injectate spread prevents intraneural injection
- Lower systemic toxicity risk: Accurate deposition avoids intravascular injection and reduces required local anesthetic volumes by up to 37% 1
For deep blocks like the lumbar plexus, where complications include retroperitoneal hematoma and renal injury, ultrasound’s safety advantages are particularly significant 1.
3. Practical and Operational Benefits
Beyond clinical outcomes, ultrasound delivers tangible practical advantages:
- Procedural efficiency: Ultrasound-guided blocks reduce performance time by 1.5-4.8 minutes compared to nerve stimulation 4
- Reduced equipment dependency: Eliminates need for nerve stimulators and their associated consumables
- Enhanced patient comfort: Faster onset times (documented improvements in 6/10 studies) minimize preoperative waiting periods 4
- Cost-effectiveness: Reduced local anesthetic requirements and decreased complication rates generate substantial savings
Table: Comparative Performance of Nerve Localization Techniques
| Parameter | Landmark-Based | Nerve Stimulation | Ultrasound Guidance |
|---|---|---|---|
| Success Rate | 40-60% | 58-93.1% | 72-98.8% |
| Procedure Time | Highly variable | Longer (reference) | 1.5-4.8 minutes faster |
| Complication Rate | High | Moderate | Significantly reduced |
| LA Volume Required | High | Moderate | Reduced (up to 37%) |
| Learning Curve | Steep | Moderate | Shallow with proper training |
4. Special Population Advantages
Ultrasound proves particularly valuable in challenging anatomical scenarios:
- Morbidly obese patients: Where surface landmarks are obscured, ultrasound provides reliable visualization of deep structures 13
- Pediatric patients: Precision dosing minimizes local anesthetic exposure in developing nervous systems
- Anatomically variant individuals: Real-time imaging accommodates anatomical variations without procedural modification
A compelling case study demonstrated successful anesthesia in a morbidly obese patient (BMI >40) using multiple ultrasound-guided blocks (TAP, LFCN, intercostobrachial) when general anesthesia posed significant risks 13.
Vendra Medical’s Vsono-PR1: Revolutionizing Ultrasound-Guided PNB
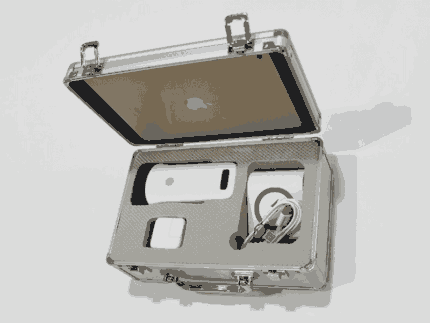
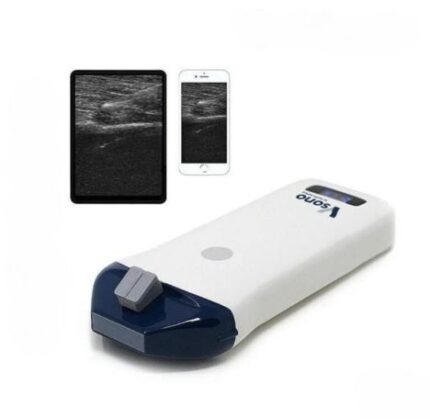
Among technological innovations in ultrasound guidance, Vendra Medical’s Vsono-PR1 Phased Array Wireless Ultrasound Scanner represents a paradigm shift in regional anesthesia practice. This cutting-edge device addresses multiple limitations of traditional ultrasound systems:
1. Unprecedented Portability
- Compact dimensions (140×60×20mm) and lightweight design (120g) enable pocket-sized mobility
- Wireless connectivity eliminates cumbersome cables that impede sterile fields
- Ideal for diverse clinical environments: OR, ER, bedside, and remote settings 11
2. Advanced Imaging Capabilities
- Phased array technology (64-channel RT) provides exceptional deep tissue penetration
- Multi-frequency options (2.5MHz, 2.8MHz, 3.6MHz) optimize imaging for superficial and deep nerve targets
- Color Doppler and PDI modes enable simultaneous vascular identification during nerve localization 11
3. PNB-Specific Features
- Puncture assist function: Provides in-plane and out-of-plane guidance with automatic vessel measurement
- Cross-platform compatibility: Seamless integration with iOS, Android, and Windows devices
- Real-time image sharing: Facilitates telemedicine consultations and educational supervision 11
4. Practical Implementation Advantages
- Rapid setup: WiFi connectivity enables scanning within 60 seconds of device activation
- Extended battery life: 1.5 hours of continuous operation accommodates multiple procedures
- Regulatory compliance: FDA and CE certifications ensure adherence to stringent quality standards
*Table: Technical Specifications of Vsono-PR1 for PNB Applications*
| Feature | Specification | Clinical Benefit |
|---|---|---|
| Scanning Mode | Electronic phased array | Enhanced deep tissue imaging |
| Display Modes | B, B/M, Color, PW, PDI | Comprehensive tissue characterization |
| Depth Range | 90-190mm | Ideal for deep nerve blocks |
| Puncture Assist | In-plane/out-of-plane guidance | Enhanced needle visualization |
| Connectivity | WiFi 802.11g/5G/450Mbps | Cable-free sterile field maintenance |
| Compatibility | iOS, Android, Windows | Flexible device integration |
Artificial Intelligence Integration: The Next Frontier
The convergence of artificial intelligence (AI) with ultrasound technology promises to further revolutionize PNB practice:
1. Automated Anatomy Recognition
- U-Net architecture algorithms achieve 73-74% accuracy in identifying key structures like the femoral nerve and TAP space 14
- Nerveblox technology provides real-time color-coded overlays differentiating nerves, vessels, muscles, and fascial planes 14
- ScanNav Anatomy PNB (Intelligent Ultrasound) offers AI-supported landmark identification for 12 common blocks 14
2. Enhanced Training and Education
- NeedleTrainer systems utilize AI color highlighting to accelerate sonoanatomy recognition 6
- Simulation platforms incorporate BPSegData (brachial plexus image datasets) to refine identification skills 14
- AI-powered feedback systems objectively assess trainee performance during simulated procedures
3. Procedural Safety Augmentation
- Magellan robotic systems enhance needle stability during precise interventions
- SmartNerve technology (Mindray) and cNerve systems (GE) integrate AI directly into ultrasound units
- Predictive algorithms alert operators to potential needle deviation or vulnerable structure proximity 14
Despite these advances, AI remains an assistive tool rather than replacement for clinician expertise. As noted in recent literature: “Will artificial intelligence replace physicians in regional block procedures? This seems unlikely. It will, however, assist them in a significant manner, contributing to better effectiveness and improved safety” 14.
Implementing Ultrasound-Guided PNB: Practical Considerations
Successful integration of ultrasound into regional anesthesia practice requires attention to several factors:
1. Training and Education
- Structured programs combining simulation training (e.g., NeedleTrainer) with supervised clinical practice 6
- Focus on developing three-dimensional spatial interpretation of two-dimensional ultrasound images
- Mastery of probe manipulation techniques: Tilting, sliding, rotation, and pressure adjustment
2. Equipment Selection
- Portable systems (e.g., Vsono-PR1) versus cart-based units based on practice needs
- Transducer selection: High-frequency linear arrays for superficial nerves, curved arrays for deeper targets
- Ergonomic considerations: Probe design, screen positioning, and cable management to prevent operator fatigue
3. Procedure Optimization
- Patient positioning: Balancing optimal ultrasound access with patient comfort
- Needle visualization techniques: Maintaining beam alignment through constant probe adjustment
- Hydrolocation: Using small saline injections to confirm needle tip position when tissue echogenicity obscures direct visualization
4. Quality Assurance
- Documentation standards: Saving representative images with procedure documentation
- Complication tracking: Systematic monitoring of block success and adverse events
- Continuous education: Incorporating new technologies like AI as they become available
Conclusion: The Future of Ultrasound-Guided Regional Anesthesia
Ultrasound guidance has fundamentally transformed peripheral nerve blockade from a blind technique to a precision intervention. The documented benefits—enhanced efficacy, improved safety, reduced resource utilization, and expanded applicability to complex patients—establish ultrasound as the gold standard for PNBs 149. Technological innovations like Vendra Medical’s Vsono-PR1 address historical limitations of ultrasound systems through wireless operation, exceptional portability, and specialized PNB features, making high-quality imaging accessible beyond traditional operating room settings.
The emerging integration of artificial intelligence promises to further democratize ultrasound expertise, providing real-time procedural guidance and enhancing anatomical recognition, particularly for less experienced operators 514. However, these technological advances complement rather than replace the essential foundation of thorough anatomical knowledge and sound clinical judgment.
As regional anesthesia continues its evolution, the synergistic combination of portable ultrasound technology, intelligent guidance systems, and clinician expertise will progressively expand access to safe, effective regional anesthesia—improving perioperative outcomes across diverse healthcare settings and patient populations worldwide.